Sydney classification- assessment of deep mural injury after endoscopic mucosal resection.
Katarzyna Pawlak, Hospital of the Ministry of Interior and Administration, Department of Internal Medicine, Cardiology, Gastroenterology and Endocrinology, Szczecin, Poland
Hospital of the Ministry of Interior and Administration, Department of Internal Medicine, Cardiology, Gastroenterology and Endocrinology, Szczecin, Poland
Classification presented by Burgess NG et al. [1] based on retrospective evaluation, clinical observations and image analysis.
It allows for the assessment of deep mural injury (DMI) after endoscopic mucosal resection (EMR) of laterally spreading colorectal lesions with the diameter > 20mm. The most important is accurate, endoscopic post-resection assessment using advanced imaging techniques, which determines further proceeding.
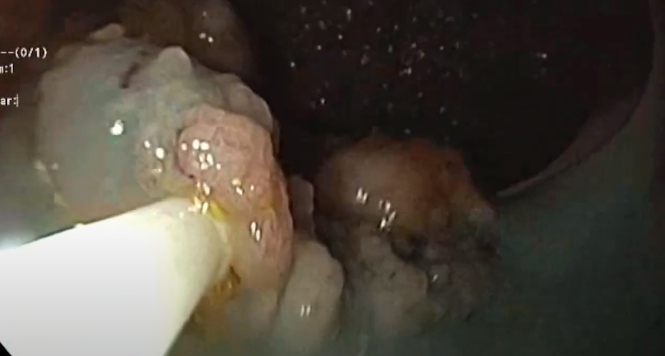
During EMR procedure, extremely important is to properly elevate and stain the lesion appropriate solutions with dyes. Injection separates the lesion from muscular layer, reducing thermal injury, risk of perforation and bleeding. Additionally, facilitates en-bloc resection in the technical aspect [2].
In turn, addition of staining agents to the injection solution, allows identifying the area of submucosal injection and distinguishing between the muscle layer and the submucosa. Morover, identification of the lateral and deep margins of the target lesion is more detailed during te whole procedure (before and after resection). Also, the staining dye may facilitate evaluation of residual lesion at the end of endoscopic resection and improve recognition of muscularis propria injury as an intraprocedural perforation [2].
Therefore, the authors used: 1 ml of 0.4% indigo carmine or methylene blue and 1 ml of 1: 10,000 adrenaline in combination with 8 ml of saline solution [1].
In this classification a proper injection is important because it allows for an accurate assessment of colon wall layers and further proceeding (clip vs. not clip vs. consult with the surgeon).
The classification is V gradual and concerns the correct view in the site after EMR where mucosa was removed correctly, up to clean / contaminated perforation [1].
The terms included in the classification:
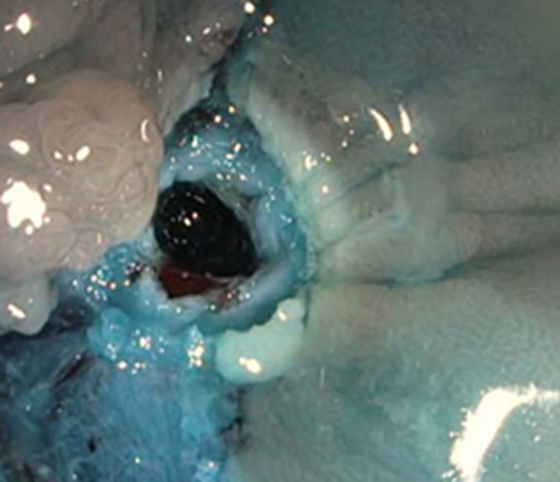
Target sign – a symptom of endoscopic resection of muscularis propria and sites of potential perforation (circularly arranged white fibers with a dark spot in the center).
Specimen sign – seen in the removed lesion, in the place of the cut seen from the bottom.
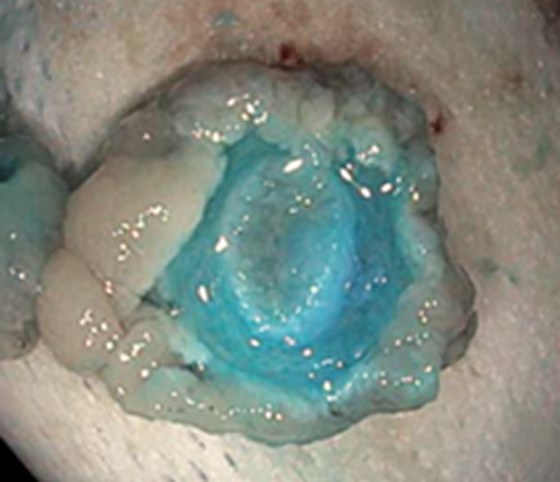
Whale sign – a circular wrap of white fibers of muscularis propria without injury (compared to the abdomen of a part of the blue whale)

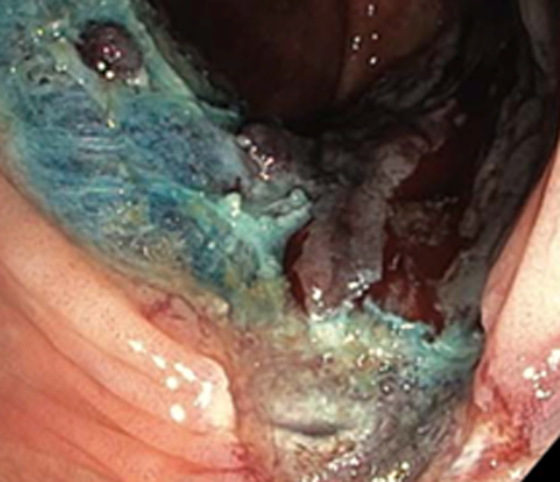
Type 0
-mucosal defect after correct resection, blue mat color with visible oblique intersecting fibers of the submucosa
– submucosal vessels may be visible, but they are not damaged


Type I
– removed submucosal layer
– white, circular muscularis propria fibers visible without damage – whale sign

Type II
– no distinction between the submucosa and muscularis propria, focal loss of the submucosal plane rising concer for mucularis propria injury
-damage of muscularis propria difficult to visualize

Type III
-damage of muscularis propria (1) visible as a target sign (2) in the resection site or specimen sign (3) visible in the removed lesion, „from the bottom“ at the cut site

Type IV
-clearly visible perforation (whole with a white cautery ring) without stool residue contamination
– perforation should be closed immediately, however, if possible, complete resection before placing the clip
– if the lesion is not completely removed before clipping, further resection attempts may be hindered by submucosal fibrosis due to the clip
Type V
-perforation contaminated with stools
– hole should be closed and surgically consulted
– surgical intervention is required adequate to the clinical condition, in case of peritonitis, peritoneal fluid, or unsuccessful endoscopic resection

Conclusions from the study [1]:
- Potential DMI (type I and II) is associated with increasing lesion size, SMF and transverse colon location.
- DMI type III–V: (target signs and perforations) are associated with en bloc resection, transverse colon location and HGD or SMIC.
- Type I injuries do not require clip placement
- DMI type III–V require closure of the injured MP
- All type II injuries should also ideally be clipped
- The majority of patients with target signs (type III DMI) can be managed with same day discharge if they are well and the injury is securely closed.
- Intraprocedural perforation occurs in 0.5% and clinically significant perforation occurs in 0.2%.
- Potentially serious DMI syndromes are not infrequent, but if recognised they may be managed safely and effectivelywithout serious clinical sequelae, in many cases on an outpatient basis.
- type III – V DMI (target sign or perforation) occurs in 3.0% and mainly affects lesions located in the transverse colon, en bloc resection, HGD and invasive cancer,
- lesions ≥25 mm removed entirely are particularly associated with a high DMI risk, therefore risk
- and the advantages of en bloc resection before EMR should be assessed.
Figures adapted from Ref. 1.
References
- Burgess NG, et al. Deep mural injury and perforation after colonic endoscopic mucosal resection: a new classification and analysis of risk factors. Gut 2016; 0:1–11.
- Castro R, Libânio D, Pita I, Dinis-Ribeiro M. Solutions for submucosal injection: What to choose and how to do it. World J Gastroenterol. 2019; 25: 777–788.
Author: Pawlak K. (1)
Hospital of the Ministry of Interior and Administration, Department of Internal Medicine,
Cardiology, Gastroenterology and Endocrinology, Szczecin, Poland