Risks of Colonoscopy: Not Just Bleeding and Perforation
Douglas K. Rex, MD, FASGE, reviewing Laanani M, et al. Am J Gastroenterol 2020 Apr.
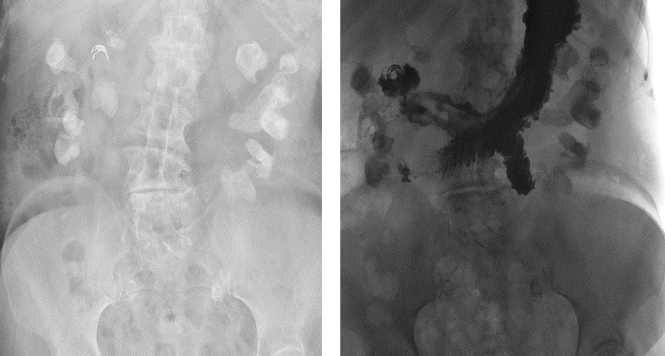
This French study evaluated 4,088,799 patients undergoing a first-time colonoscopy during a 6-year interval. Patients with inflammatory bowel disease, colorectal cancer, or complicated diverticular disease were excluded. For every 10,000 procedures, the 5-day rate of shock was 2.8, myocardial infarction (MI) was 0.87, stroke was 1.9, pulmonary embolus was 2.9, acute renal failure was 5.5, and urolithiasis was 3.3. More than 95% of patients with these complications did not have concomitant perforation or bleeding. Standardized incidence ratios were increased for all, ranging from 3.3 for MI to 15.8 for shock. Thirty-day mortality ranged from 2.2 per 1000 cases for urolithiasis to 268 per 1000 for shock. Age and comorbidities were risk factors for systemic adverse events. Previous stroke, MI, renal disease, and urolithiasis were all risk factors for the same events. Patients with diabetes or liver disease were at increased risk of renal systemic adverse events; metastatic cancer was a risk factor for multiple systemic adverse events.

COMMENTThese findings remind us that colonoscopy is a procedure that involves more than examining the colon and removing polyps. There is bowel preparation, sedation, and procedural stress. These risks should be considered in patients with advanced age and comorbidities.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Laanani M, Weill A, Carbonnel F, Pouchot J, Coste J. Incidence of and risk factors for systemic adverse events after screening or primary diagnostic colonoscopy: a nationwide cohort study. Am J Gastroenterol 2020;115:537-547. (https://doi.org/10.14309/ajg.0000000000000574)