Epinephrine Caused Increased Postprocedural Pain When Used for Colorectal EMR
Douglas K. Rex, MD, MASGE, reviewing Rex DK, et al. Gastrointest Endosc 2021 Dec 9.
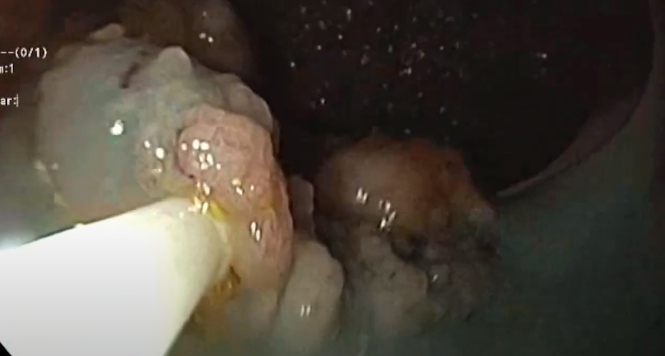
Including epinephrine in the submucosal injectate for endoscopic mucosal resection (EMR) varies among endoscopists – some endoscopists prefer epinephrine, whereas others do not. Of those who utilize epinephrine, concentrations used range from 1 in 10,000 to 1 in 500,000, according to published literature.
In a randomized controlled trial of 20 patients with large (mean size >40 mm) laterally spreading colorectal lesions, the inclusion of epinephrine at 1 to 200,000 dilution was associated with a higher pain score on a 100-mm visual analog scale at 30 minutes (47 vs 14; P=.022) and 60 minutes (44 vs 13; P=.035). In addition, the duration of stay in the recovery room was longer in the epinephrine group (68 vs 53 minutes; P=.034).

COMMENTThis study originated from anecdotal observations that epinephrine used for EMR of very large lesions appeared to be associated with greater postprocedural discomfort and nausea, possibly related to temporary ischemia. If this occurs with epinephrine use, and the defect appears normal, it seems reasonable to wait before performing imaging because the pain associated with epinephrine typically resolves within 2 to 3 hours. It’s currently unclear whether this effect could be related to inadvertent intraperitoneal or intramuscular injection.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Rex DK, Lahr RE, Peterson M, Vemulapalli KC. Impact of including epinephrine in the submucosal injectate for colorectal endoscopic mucosal resection on postprocedural pain: a randomized controlled trial. Gastrointest Endosc 2021 Dec 9. (Epub ahead of print) (https://doi.org/10.1016/j.gie.2021.11.043)