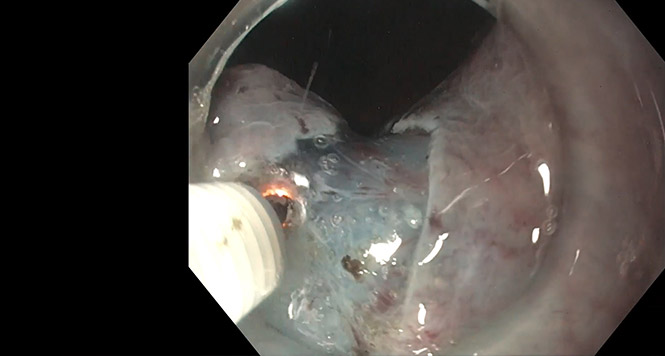
Endoscopic Submucosal Dissection for Early Colorectal Cancer and High-Risk Surgery: Okay to Not Operate
Douglas K. Rex, MD, MASGE, reviewing Spadaccini M, et al. Gut 2022 Jan 20.
This study investigated outcomes in patients who underwent endoscopic submucosal dissection (ESD) for T1 colorectal cancer (CRC) and then had adverse histologic features that predict lymph node involvement (poor differentiation, submucosal invasion >1000 microns, lymphovascular invasion, intermediate- or high-grade tumor budding, or positive resection margins [R1]). In this multicenter, multinational study, 604 patients underwent ESD for submucosal invasion, but 207 resulted in noncurative resections (adverse histology). Of the patients who had noncurative ESD, 61% received subsequent surgical treatment and 39% were followed up by endoscopy without surgery.
Among 126 patients who underwent surgery, 19.8% had histologic evidence of nodal involvement (15.1%) and/or residual neoplasia in the bowel (7.1%). Only rectal location (and not R0 resection) was associated with residual disease. Five patients in the surgical group developed recurrent cancer, and 3 died of CRC. In general, R1 resection did not predict residual disease.
The outcomes in the endoscopic group were the main interest of the study. Patients in the endoscopic follow-up group were older than those in the surgical group (mean age, 70 vs 66 years, respectively), had higher Charleston Comorbidity Index scores (median, 5 vs 3), and were more likely to have rectal cancer. Patients in the endoscopic follow-up group also had higher overall mortality (hazard ratio, 3.95), but the causes were unrelated to CRC.

COMMENTIncreasing evidence suggests that deep submucosal invasion (>1000 microns) is not an independent predictor of lymph node metastases in the absence of other adverse histologic predictors. These data also question the importance of R1 resection as a predictor of residual disease after ESD. These data generally support surgical resection after ESD for T1 CRC and adverse histologic features in good surgical candidates. Although the endoscopic follow-up group had some recurrences with further follow-up, the high mortality from causes other than CRC and the lack of any CRC mortality during follow-up suggest that nonoperative management is best after endoscopic resection of T1 CRC when patients are high risk for surgery, even when they have unfavorable histologic features.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Spadaccini M, Bourke MJ, Maselli R, et al. Clinical outcome of non-curative endoscopic submucosal dissection for early colorectal cancer. Gut 2022 Jan 20. (Epub ahead of print) (https://doi.org/10.1136/gutjnl-2020-323897)