Continuing Antithrombotics Substantially Increases Risk of Delayed Bleeding After Colorectal ESD
Douglas K. Rex, MD, MASGE, reviewing Kawasaki K, et al. J Gastroenterol Hepatol 2023 Feb 19.
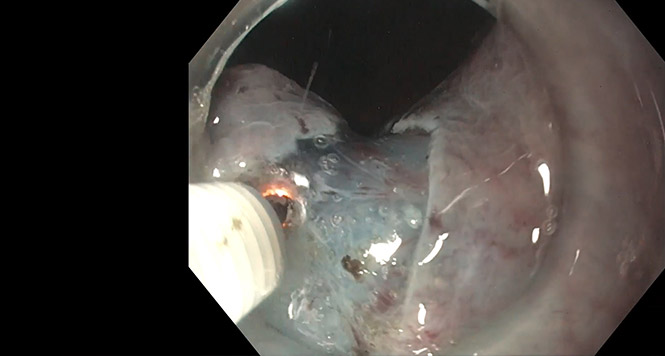
In this retrospective study from Japan, researchers compared delayed bleeding rates for 82 patients who underwent ESD while continuing antithrombotic medications versus 386 patients without the medications.
All patients were hospitalized for up to a week, and none had closure of the ESD defect. After propensity score matching, the rate of delayed bleeding with continuation of antithrombotics was 21.6% versus 5.4% without antithrombotics.
Propensity score matching showed that the risk of delayed bleeding increased with low-dose aspirin (odds ratio [OR], 9.4), direct oral anticoagulants (OR, 10.8), and warfarin (OR, 7.8), but not thienopyridines, though numbers were small in each group.

COMMENTAn interesting aspect of these data is the high risk of post-ESD bleeding among patients taking low-dose aspirin, which is continued for many endoscopic procedures in the U.S. These data indicate that continuation of antithrombotics during colorectal ESD is feasible (when clinically essential), but it likely warrants closure of the ESD defect given that, in the U.S., patients are not observed in the hospital for long periods.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Kawasaki K, Torisu T, Esaki M, et al. Continuous use of antithrombotic medications during peri-ESD period for colorectal lesions: a propensity score matched study. J Gastroenterol Hepatol 2023 Feb 19. (Epub ahead of print) (https://doi.org/10.1111/jgh.16149)