Are Anesthesia Specialists Necessary for Complex Colorectal Endoscopic Mucosal Resections?
Douglas K. Rex, MD, MASGE, reviewing Gupta S, et al. Endosc Int Open 2023 Sep 25.
Sedation practice for endoscopy varies widely in the United States. One model is to use anesthesia specialists to administer propofol for complex endoscopic procedures, such as endoscopic retrograde cholangiopancreatography, endoscopic ultrasound, and endoscopic submucosal dissection.
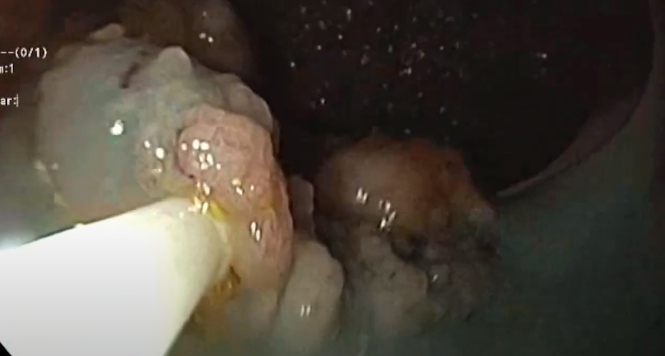
In this report, investigators describe the outcomes of physician-administered balanced propofol sedation (along with the use of opioids and benzodiazepines) for endoscopic mucosal resection (EMR) of nonpedunculated colorectal lesions ≥20 mm in size. Over a 4-year interval, 700 patients underwent EMR, with 638 receiving propofol sedation administered either by an advanced endoscopy fellow or the consulting gastroenterologist supervising the procedure.
During the interval, the use of this model increased from 87.1% to 95.8%, with the remainder of patients receiving sedation from an anesthetist. Compared with patients who received sedation administered by an anesthetist, patients receiving balanced propofol sedation given by an endoscopist had a median age 4 years younger and a lower Charlson Comorbidity Index. Before and after propensity score matching, there was no difference between the endoscopist-sedated and anesthetist-sedated patients in periprocedural events, such as hypotension, hypertension, arrhythmia, and hypoxia, and there was no difference in other adverse events, including immediate or delayed adverse events of the procedure, need for hospitalization, technical success of the procedure, and recurrence rates at first follow-up. This was also true for more complex resections, including those involving the ileocecal valve, anorectal junction, and a prior attempt at resection.

COMMENTIn the United States, more practices are converting to routine use of propofol administered by anesthetists for all procedures, driven largely by patient satisfaction, endoscopist convenience, financial incentives, and, in many cases, institutional requirements that are also often linked to financial incentives. However, it is worth remembering that evidence of improved outcomes from the administration of anesthesia by anesthetists is scant and that, for colonoscopy, propofol sedation is associated with an increased risk of aspiration.
These data indicate that complex colorectal EMR is not necessarily one of the advanced procedures requiring an anesthetist. However, this model in which two endoscopists are available, one to perform the procedure and one to sedate the patient, is not generally feasible in American practice. Certainly, considerable evidence indicates that trained registered nurses can safely administer balanced propofol sedation under the supervision of an endoscopist performing the procedure, and there is no reason to believe endoscopist-directed nurse-administered balanced propofol sedation (also now seldom considered feasible or advisable in the U.S.) could not be safely extended to colorectal EMR.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Gupta S, Kurup R, Shahidi N, et al. Safety and efficacy of physician-administered balanced-sedation for the endoscopic mucosal resection of large non-pedunculated colorectal polyps. Endosc Int Open 2023 Sep 25. (Epub ahead of print) (https://doi.org/10.1055/a-2180-8880)