Endoscopic Management of Perforations: AGA Clinical Practice Update
Vanessa M. Shami, MD, FASGE, reviewing Lee JH, et al. Clin Gastroenterol Hepatol 2021 Jul 1.
A practice update from the American Gastroenterological Association used expert review and focus on methodologies to develop best practice recommendations for the management of endoscopic perforations. Below are notable points from all 16 recommendations:
- Risks, including perforation and other AEs, should be thoroughly discussed with patients (and preferably families) before endoscopic procedures.
- A perforation site should be kept free of luminal contents, and patients may need to be turned so the site is in a nondependent position. Carbon dioxide use is recommended, especially for high-risk procedures. Surgical consultation should be considered in all patients.
- In upper GI perforations, patients should be given nothing by mouth, treated with broad-spectrum antibiotics, and potentially admitted. Before resuming per-oral intake, consideration should be given to performing a water-soluble upper GI study to confirm there is no leak.
- Primary closure of esophageal and gastric perforations should be attempted using through-the-scope clips (TTSCs) or over-the-scope clips (OTSCs) for perforations <2 cm, or endoscopic suturing for those >2 cm. Esophageal stenting should be reserved when primary closure is not feasible.
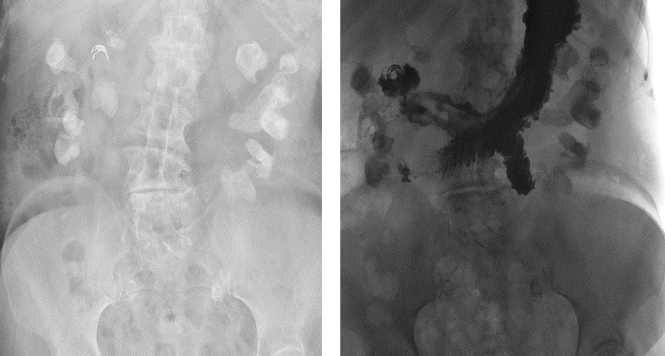
- In duodenal perforations, surgical consult should not be delayed for a large (>3 cm) type 1 perforation, regardless of whether endoscopic closure is attempted. For type 2 (retroperitoneal), recognition of perforation is key and closure with TTSCs and/or bile duct placement of self-expanding metal stents should be attempted. Duodenal resections should be performed by physicians proficient in advanced resection techniques.
- For colonic perforations, the sigmoid is the most common area of perforation in diagnostic colonoscopies and can be closed by TTSCs or OTSCs. On the right side of the colon, TTSCs are the most feasible.
- Direct surgical referral is important in patients with hemodynamic instability, delayed perforation, or peritonitis.
- Documentation of AEs and communication with the patient and family, as well as the appropriate hospital or facility reporting body, are imperative.

COMMENTThese authors have highlighted the important considerations before, during, and after endoscopic procedures in patients at risk for perforation. Communication, teamwork, and recognizing one’s strengths and limitations as an endoscopist are key for the optimal care and management of patients.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Lee JH, Kedia P, Stavropoulos S, Carr-Locke D. AGA clinical practice update on endoscopic management of perforations in gastrointestinal tract: expert review. Clin Gastroenterol Hepatol 2021 Jul 1. (Epub ahead of print) (https://doi.org/10.1016/j.cgh.2021.06.045)