Achalasia — place of endoscopic therapy in the light of the first long-term data for POEM
Till Wehrmann, Wiesbaden
| Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years |
| Yuki B Werner, Guido Costamagna, Lee L Swanström, Daniel von Renteln, Pietro Familiari, Ahmed M Sharata, Tania Noder, Guido Schachschal, Jan F Kersten, Thomas Rösch |
Background
The recently developed technique for peroral endoscopic myotomy (POEM) has been shown to be effective in several short-term studies. Longer termoutcome data are largely non-existent.
Objective
To systematically report clinical outcome with a minimum post-POEM follow-up of 2 years.
Design
All patients treated consecutively by POEM for achalasia at three centres were retrospectively analysed, with a minimum follow-up of 2 years. The main outcome was the rate of POEM failures (Eckardt score >3) related to follow-up time.
Results
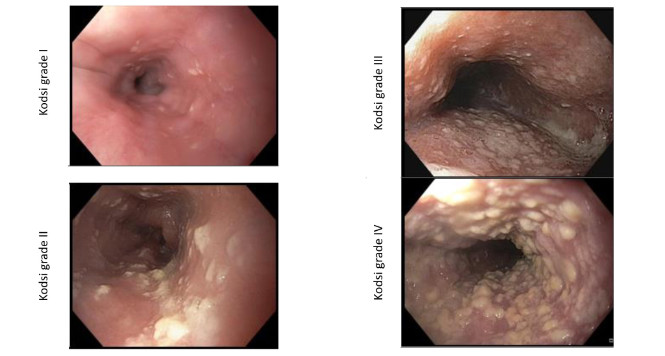
Of 85 patients treated, five (5.9%) cases were excluded due to protocol violation or loss to follow-up; the remaining 80 patients (mean age 44.9 years, 54% men) were followed clinically for 29 months (range 24–41). Initial clinical response was observed in 77 cases (96.3%). Clinical recurrences (later failures) were seen in a further 14 cases (17.7%), accounting for a total failure rate of 21.5%. In a multivariate analysis, age and endoscopic reflux signs were independent predictors of treatment success. Of the 17 failures, eight were among the first 10 cases treated in the participating centres. Reflux-associated sequelae included one case of a severe reflux-associated stricture requiring dilatation, and two patients with minor transient Eckardt score elevations curable by proton pump inhibitor (PPI) treatment. Endoscopic signs of reflux oesophagitis, mostly Los Angeles grade A/B, were seen in 37.5% (37/72) at the 2-year control.
Conclusions
In this multicentre retrospective analysis, a high initial success rate of POEM is followed by a midterm recurrence rate of 18%. Reflux oesophagitis, albeit mild, is frequent and should probably be treated by regular low-dose PPI therapy.
What you need to know
Achalasia is a rare neuromuscular disease of unclear etiology that probably has a genetic background. The precise etiopathogenesis of achalasia is still unclear. Above all, neurodegenerative changes in the myenteric plexus in the esophagus can be demonstrated; in addition, there is evidence for a (probably clinically irrelevant) systemic manifestation of the disease in the entire gastrointestinal tract, also accompanied by changes in the central nervous system (1, 2). Despite earlier speculation about possible viral infections as the cause of achalasia, evidence of a genetic background for the disease has recently been presented (1, 2). Pathophysiologically, the disease is characterized by a lack of swallowing-reflex relaxation of the lower esophageal sphincter (LES) and limited propulsive peristalsis in the smooth-muscle parts of the tubular esophagus (1). A causal approach to treatment is not yet possible, and the great majority of treatment options are aimed at weakening/eliminating the lower esophageal sphincter in order to compensate for its lack of swallowing-reflex relaxation (1–3). According to Pandolfino et al. (4), high-resolution manometry can distinguish between three subtypes of achalasia, with type III in particular (earlier known as “vigorous achalasia”) probably benefiting least from all of the therapeutic procedures currently available. The symptomatic picture of achalasia is best quantified for research purposes using the Eckardt score (1).
To date, only noncausal, symptom-oriented treatments have consequently been available. In order of invasiveness, these include botulinus toxin (BTX) injection (procedure duration 10 min, with sedation, mortality zero); pneumatic dilation (PD; procedure duration 15–20 min, with sedation, mortality ca. 0.1%); and peroral endoscopic myotomy (POEM; procedure duration 90–120 min, with general anesthesia, mortality not clear but ca. 0.1%). The surgical alternative is laparoscopic cardiomyotomy (procedure duration 120–240 min, with general anesthesia, mortality ca. 0.3%). Whereas BTX injection with one application (response rate ca. 80–90%) only produces short-term symptomatic relief (ca. 4–6 months) and is therefore only suitable — with repeated application — for patients with limited life expectancy, PD provides symptomatic improvement for 5–10 years in approximately 40–60% of cases. By contrast, the 5–10-year success rates with laparoscopic cardiomyotomy are ca. 80%, and this procedure is therefore the standard treatment for younger patients in particular. In a randomized comparison over a 2-year period, however, cardiomyotomy and PD were found to be equally effective.
In principle, botulinus toxin leads to inhibition of acetylcholine release at the motor end plate, and when applied locally (e.g., with endoscopic visualization at the cardia), it can therefore limit muscle function. However, due to new germination of intact neurons (not blocked by BTX), functionally effective reinnervation occurs after a few months. For example, after a single application at the cardia, effects on the LES lasting 4–6 months were observed (2). Reinjections are possible, and in individual cases (e.g., in elderly patients), symptomatic relief lasting several years can be observed (2). Side effects are not expected, but the treatment procedure has not been approved for use in the esophagus.
Pneumatic dilation (PD) leads to tearing of the LES musculature, usually with local hematoma formation. The principal complication is therefore perforation, which is reported with a frequency of 1–7% of cases. However, appreciable mortality is now lo longer observed. Postinterventional symptomatic improvement (Eckardt score < 3) is observed in 80–95% of cases (1, 2). However, the recurrence rate is high, at 40–60% within 5–10 years (1). Younger patients in particular, and those with insufficient pressure reduction at the LES (residual pressure > 15 mmHg) have a poorer prognosis (1, 2). Repeat dilation can be carried out, and this was therefore the method of choice in the prelaparoscopic era.
Laparoscopic cardiomyotomy also leads to controlled but better destruction of the LES; in addition, a longitudinal myotomy is carried out in the lower third of the esophagus. The acute symptomatic benefit is usually > 90% (1). In studies reporting long-term follow-up periods, success rates of 70–80% after 5 years are reported, and younger patients (< 40 y) in particular have good results. In a prospective and randomized multicenter study in Europe, however, the results after PD or cardiomyotomy were equivalent after 2 years (each with sustained symptomatic improvement in 86% of cases, both after PD and after surgery) (5).
In peroral endoscopic myotomy (POEM), the esophageal sphincter muscles are transected in the middle and distal area over a length of ca. 8–11 cm. In addition, the longitudinal muscles are also usually transected, at least in the area of the cardia. In laparoscopic myotomy, the longitudinal and annular muscles are usually transected over a length of 8 cm in the esophagus, and the incision is extended by 3–4 cm distal from the cardia towards the stomach; in POEM, this length is usually 2 cm. Laparoscopic myotomy is usually supplemented with placement of a 180° or 360° fundoplication, but this has not yet been a standard in POEM procedures.
POEM was first described by Pasricha et al. in animal experiments (6). Following lifting of the submucosa with an injection, an incision into the mucosa is made and the submucosal space is then tunneled longitudinally in the distal direction with the endoscope, up to just less than 2 cm distal to the cardia. A myotomy of the longitudinal muscles in the area of the cardia is then carried out, up to ca. 1–2 cm aboral from the incision in the tubular esophagus. This results in a myotomy that is usually at least 10 cm long (usually ca. 11–12 cm), although myotomy lengths of up to 25 cm have been reported (3). Finally, the incision site is closed with clips. The procedure is usually carried out with the patient under general anesthesia, and instead of air insufflation, CO2 insufflation is used to minimize the extent of pneumomediastinum. In a study comparing POEM with laparoscopic cardiomyotomy, the radiographic findings showed that the two procedures were equally effective in relation to functional parameters (7), so that the lack of a consistent longitudinal myotomy in the POEM procedure is not associated with poorer effectiveness, at least in the short term. In an initial study by Inoue et al. (8), significant reductions in the dysphagia score and LES pressure were documented in 17 patients. In the majority of the published studies (see below), subcutaneous emphysema was reported in ca. 15% of cases and capnoperitoneum was noted in half of the cases. Overall, relevant mediastinitis was documented in ca. 0.2% of the patients (managed conservatively and with drains), but no mortality has so far been reported (2, 3). There is a learning curve involved in achieving the optimal results, and it is assumed that adequate competence is acquired after 20 procedures (9). This method is the first procedure from the range of natural orifice transluminal endoscopic surgery (NOTES) techniques that has become genuinely established in centers all over the world.
The acute success rates with POEM can be defined by a reduction in clinical symptoms (reduction in the Eckardt score < 3 points), a reduction in lower esophageal sphincter pressure by ca. > 50%, and an improvement in the cardia width and retention height in esophageal barium swallows on radiography. The published response rates here are 80–100% over a follow-up period of 3–12 months. The following table shows the acute results from full-text studies published to date on the POEM procedure in patients with achalasia.
| Author | n | Eckardt score (points) before/after |
LES pressure (mmHg) before/after |
Response rate (%) |
Follow-up (months) |
|---|---|---|---|---|---|
| Inoue, Endoscopy 2010 |
17 | 10/1 | 52/19 | 100 | 5 |
| Swanström, J Am Coll Surg 2011 |
18 | 6/0 | 45/17 | 94 | 6 |
| Costamagna, Dig Liver Dis 2012 |
11 | 7/1 | 45/17 | 100 | 3 |
| Von Renteln, Am J Gastro 2012 |
16 | 8/1 | 27/12 | 94 | 3 |
| Teitelbaum, Surgery 2013 |
41 | 7/1 | 22/9 | 92 | 12 |
| Von Renteln, Gastroenterology 2013 |
70 | 7/1 | 28/9 | 82 | 12 |
| Minami, Dig Endosc 2014 |
28 | 7/1 | 71/21 | 100 | 16 |
No data have been published to date on longer-term remission rates. In a recent retrospective analysis from three centers (Hamburg, Portland, and Rome), the clinical efficacy of POEM over a follow-up period of just under 2.5 years (24–41 months) was reported for 80 patients. The acute success rate was 96%, with a recurrence rate of 18% of the patients during the 2-year follow-up period. In addition, clinical reflux symptoms were observed in around one-third of the cases and reflux esophagitis was detected in 37.5% of the patients at the 2-year check-up; one patient developed a peptic stricture. The efficacy of POEM appears to be quite comparable with that of laparoscopic cardiomyotomy, but due to the lack of antireflux plasty, postinterventional reflux problems need to be taken into account.
A retrospective analysis of the research data on POEM for achalasia by Werner et al. (10) provides the first data with a methodologically sound follow-up period of more than 1 year. The results confirm that there is a learning curve (approximately half of the patients who developed recurrences were among the first 10 cases in each of the participating centers). The medium-term response rate of 80% is almost comparable with cardiomyotomy (and probably also with pneumatic dilation). Clinically relevant reflux can be expected in one-third of the patients, slightly higher than after cardiomyotomy or PD. However, the reflux can usually be managed with drug treatment. New Barrett’s metaplasia was histologically confirmed in two of 80 patients (with endoscopically ultrashort or undetectable Barrett’s segments); one patient had to undergo bougienage for a peptic stricture. Either routine PPI medication or pH-metry after POEM treatment is therefore useful. A subanalysis for predictive factors for a response to POEM showed that older patients and those with reflux symptoms had more favorable outcomes after POEM. POEM may be able to close a gap here between cardiomyotomy (with the best results in patients aged < 40), PD (with the best results in patients aged > 60), and BTX therapy (optimally when there is a life expectancy of 2–5 years). The future of achalasia treatment will continue to be exciting.
References
- Eckardt AJ, Eckardt VF. Treatment and surveillance strategies in achalasia: an update. Nat Rev Gastroenterol Hepatol 2011; 8: 311-319.
- Mueller M, Eckardt AJ, Wehrmann T. An endoscopic approach to achalasia. Wrld J Gastrointest Endosc 2013; 5:379-390.
- Tantau M, Crisan D. Peroral endoscopic myotomy: Time to change our opinion regarding the treatment of achalasia ? Wrld J Gastrointest Endosc 2015; 7: 237-46.
- Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 2008; 135:1526-1533.
- Boeckxstaens GE, Annese V, de Varannes SE et al. European Achalasia Trial Investigators. Pneumatic dilation versus laparoscopic Heller myotomy for idiopathic achalasia. N Engl J Med 2011; 364: 1807-1816.
- Pasricha PJ, Hawari R, Ahmed I et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 2007; 39:761-764.
- Teitelbaum EN, Rajeswaran S, Zhang R et al. Peroral oesophageal myotomy (POEM) and laparoscopic Heller myotomy prodruce a similar short-term anatomic and functional effect. Surgery 2013; 154: 893-897.
- Inoue H, Minami H, Kobayashi Y et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010; 42:265-271.
- Kurian AA, Dunst CM, Sharata, A et al. Peroral endoscopic myotomy: defining the learning cirve. Gastrointest Endosc 2013; 77: 719-725.
- Werner YB, Costamagna G, Swanstroem LL et al. Clinical response to peroral endoscopic myotomy in patients with idiopathic achalasia at a minimum follow-up of 2 years. Gut 2015; in press