Achalasia: Chicago Classification
Dr. Yuki Werner
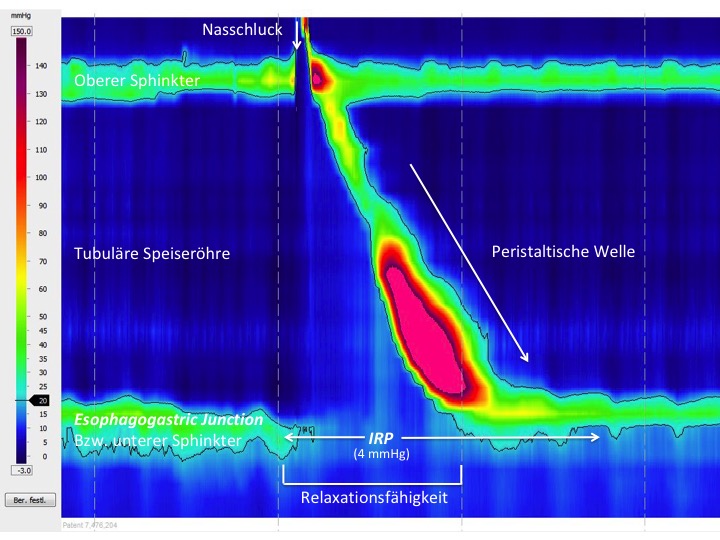
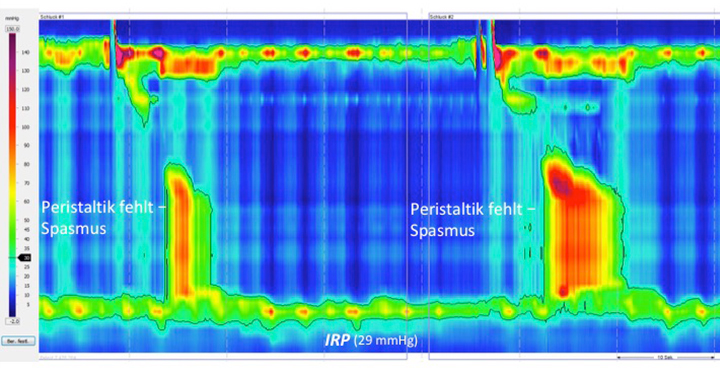
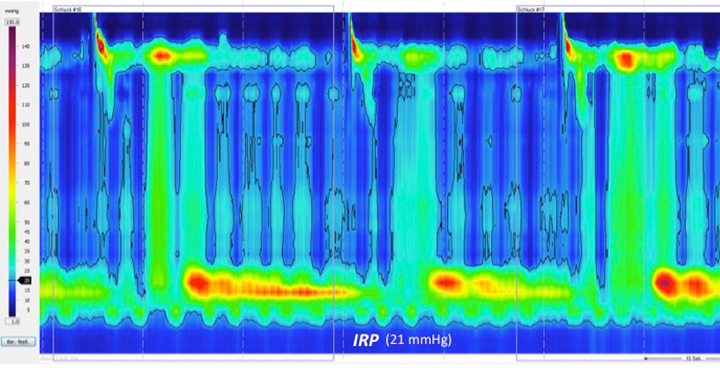
Achalasia is one of the differential diagnoses in patients with symptoms of dysphagia. High-resolution (HR) manometry is now regarded as the diagnostic gold standard for disturbances of esophageal motility. Manometry not only establishes the diagnosis, but also allows the condition to be classified into subtypes that may be important for the subsequent treatment. Three subtypes of achalasia are distinguished in what is known as the Chicago classification. Achalasia is present when relaxation of the lower esophageal sphincter during swallowing is limited or absent and propulsive peristalsis in the tubular esophagus is either not present or has been replaced with a premature spasm. In high-resolution manometry, it is therefore necessary to follow a standardized procedure (10 wet swallows) and initially measure the integrated relaxation pressure (IRP; normal value < 15 mmHg) at the esophagogastric junction (EGJ), as well as assessing the peristalsis pattern.
Normal findings:
Type I achalasia:

Type II achalasia:

Type III achalasia:
The classification is ideally carried out in patients with no previous treatment. Particularly in the clinical context and with increasing experience, it is important to assess and treat variations, such as atypical forms of achalasia, and above all forms that represent pseudo-achalasia in malignant diseases.
Example case of pseudo-achalasia:
This is a case of pseudo-achalasia – in this patient, the dysphagia symptoms were due to a distal esophageal carcinoma with submucosal growth. New-onset, rapidly progressive dysphagia and substantial weight loss, as well as the manometric findings, showing apparent swallowing-induced relaxation, led to a second endoscopic examination with histological confirmation of the diagnosis.
References
- Roman S, Huot L, Zerbib F et al. High-Resolution Manometry Improves the Diagnosis of Esophageal Motility Disorders in Patients With Dysphagia: A Randomized Multicenter Study. Am J Gastroenterol. 2016;111:372-80.
- Kahrilas PJ, Bredenoord AJ, Fox M et al. The Chicago Classification of esophageal motility disorders, v3.0.Neurogastroenterol Motil. 2015;27:160-74.
- Pandolfino JE, Kwiatek MA, Nealis T et al. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135:1526-33.