Transcutaneous SpyGlass-guided rendezvous
Dr. Christian Dietrich, Dr. Erik-Sebastian Fuchs, Prof. Dr. Ralf Jakobs, Dr. Christian Dietrich
Medizinische Klinik C - Klinikum der Stadt Ludwigshafen
Introduction and case report
Achieving sustained biliary drainage in patients with cholestasis or cholangitis often represents a turning-point in the treatment of malignant and infectious diseases with hepatobiliary involvement. In this case — a 76-year-old woman with carcinoma of the pancreatic head, with hepatic metastases — endoscopic retrograde access was not possible, due to tumor tissue extending as far as the hepatic portal. Alternative procedures include percutaneous transhepatic cholangiography and drainage (PTCD) or endoscopic ultrasound–guided drainage techniques, with the advantages and disadvantages associated with each [1]. (For further information on this, reference may be made to the video contribution by B. Walter and A. Meining from Ulm in Endoscopy Campus [2]).
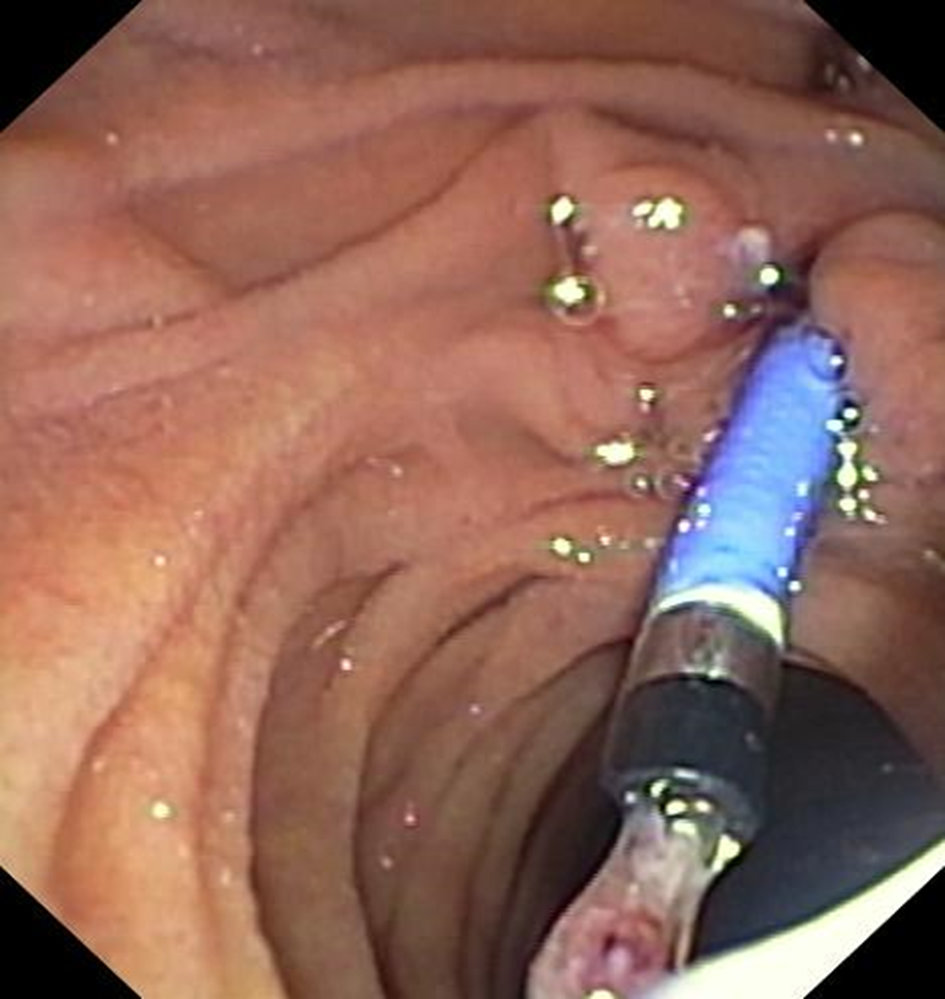
Transcutaneous bile drainage is possible after PTCD, but it is associated with a complication-prone loss of fluid and electrolytes and is susceptible to stent dislocation. For longer-term treatment, the aim must be to internalize the drainage from a transcutaneous to an intestinal route. This was not achieved in the present case even after the use of different catheters and various wires for guidance. In the following illustrations, we present an advanced technique with transcutaneous SpyGlass DS II–guided biliary drainage using a rendezvous technique, ending with successful placement of a metal stent. In this case, the procedure enabled the patient to undergo outpatient chemotherapy.
A special percutaneous version of the SpyGlass has recently been presented. In the present case, the regular SpyGlass DS II was used — with the advantage over conventional cholangioscopes that it only requires a small biliocutaneous tract diameter (12 versus 14–18 Fr).


References
- Duan F, Cui L, Bai Y et al. Comparison of efficacy and complications of endoscopic and percutaneous biliary drainage in malignant obstructive jaundice: a systematic review and meta-analysis. Cancer Imaging. 2017 Oct 16;17(1):27. doi: 10.1186/s40644-017-0129-1.
2. Walter B, Meining A. Transgastric biliary drainage with metastatic gallbladder cancer [video, Internet]. Munich: Endoscopy Campus GmbH; 2016 Nov 12. Available at: https://www.endoscopy-campus.com/en/lehrvideo/transgastric-biliary-drainage-with-metastatic-gallbladder-cancer/. Accessed 2021 Jun 29.




