Metal stents for pancreatic cyst drainage – equivalent success, more complications?
Thomas Rösch, Hamburg
Gastrointest Endosc 2017 July 14. [Epub ahead of print]
| ORIGINAL ARTICLE EUS-guided drainage of perinpancreatic fluid collections with lumen-apposing metal stents and plastic double-pigtail stents: comparison of efficacy and adverse event rates |
| Gabriel D. Lang, MD,1 Cassandra Fritz, MD,2 Trisha Bhat,3 Koushik K. Das, MD,1 Faris M. Murad, MD,4 Dayna S. Early, MD,1 Steven A. Edmoundowicz, MD,5 Vladimir M. Kushinir, MD,1 Daniel K. Mullady, MD1 |
| St. Louis, Missouri, Chicago, Illinois, Aurora, Colorado, USA |
Background and Aims
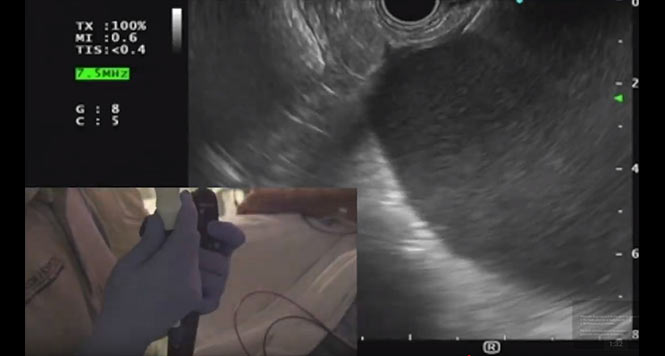
Transmural drainage with double-pigtail plastic stents (DPPSs) was the mainstay of endoscopic therapy for symptomatic peripancreatic fluid collections (PPFCs) until the introduction of lumenapposing covered self-expanding metal stents (LAMSs). Cur-rently, there are limited data regarding the efficacy and adverse event rate of LAMSs compared with DPPSs.
Methods
A retrospective analysis of EUS-guided PPFC drainage at a single tertiary care center between 2008 and 2015 was performed. Patients were classified based on drainage method: DPPSs and LAMSs. Adverse event rates, unplanned endoscopic procedures/necrosectomies, and PPFC resolution within 6 months were recorded. Significant bleeding was defined as necessitating transfusion or requiring endoscopic treatment/radiographic embolization. Subsequent endoscopic procedures were defined as un-planned procedures; stent removals were excluded.
Results
A total of 103 patients met inclusion criteria (84 DPPSs, 19 LAMSs). PPFCs were clas-sified as walled-off necrosis (WON) in 23 (14 DPPSs, 9 LAMSs). There were signifi-cantly more bleeding episodes in the LAMS group (4 [19%]: 2 splenic artery pseu-do-aneurysms, 1 collateral vessel bleed, 1 intracavitary variceal bleed; P Z .0003) than in the DPPS group (1 (1%]: stent erosion into the gastric wall). One perforation occur-red in the DPPS group. Unplanned repeat endoscopy was more frequent in the LAMS group (10% vs 26%, PZ.07). Among retreated LAMS patients in withWON, 5 (56%) had obstruction by necrotic debris. In patients for whomfollow-up was available, 67 of 70 (96%) with DPPSs and 16 of 17 (94%) with LAMSs had resolution of PPFCs within 6 months (P Z .78).
Conclusions
DPPSs and LAMSs are effective methods for treatment of PPFCs. In our cohort, use of LAMSs was associated with significantly higher rates of procedure-related bleeding and greater need for repeat endoscopic intervention.
Gut 2016 August 31 [Epub ahead of print]
| Gut Online First, Published on August 31, 2016 as 10.1136/gutjnl-2016-312812 Lumen-apposing metal stents (LAMS) for pancreatic fluid collection (PFC) drainage: may not be business as usual |
| Ji Young Bang, Muhammed Hasan, Udayakumar Navaneethan, Robert Hawes, Shyam Varadarajulu |
Message
Lumen-apposing metal stents (LAMS) have been recently developed to improve treat-ment outcomes in the endoscopic management of pancreatic fluid collections (PFC), particularly in walled-off necrosis (WON), to facilitate better drainage of necrotic con-tents and minimise the risk of perforation and peritoneal leakage. In an ongoing rando-mised trial, we observed serious adverse events that included delayed bleeding, buried stent syndrome and biliary stricture that necessitated a change in the management protocol for patients with PFC treated with LAMS.
What you should know about these papers
Endosonographic drainage of pancreatic cysts is currently regarded as the standard throughout the world, in comparison with other treatments (such as percutaneous drainage or surgery). Two plastic stents, usually the pigtail type, are placed for drainage in most cases and are left in situ for at least several weeks. An older randomized trial stated that the plastic stents should be left in place for up to a year in order to obtain better drainage results [1] — an approach that has obviously not been adopted by many in clinical practice.
Metal stents were introduced many years ago in order to provide better and more consistent drainage — conventional fully covered biliary stents initially, and later special yo-yo–type stents (also fully covered), of which the so-called Hot Axios is the most prominent and best-marketed stent type. It is relatively easy and quick to place and is expected to achieve rapid evacuation of cyst fluid. Particularly for infected cysts and necroses (called “walled-off necroses,” WONs), this stent appears to be especially useful, as it provides wide lumen access (10 or 15 mm). Experts have already welcomed this stent with great enthusiasm — as often occurs before good, prospective, or even randomized data become available (“our paper suggests that the AXIOS stent is an innovative therapeutic approach for PFC drainage with excellent efficacy, safety, and relatively few adverse outcomes”) [2]. As usual nowadays, there is also already a “meta-analysis” comparing metal and plastic stents that reports similar efficacy and complication rates [3], without a single randomized trial being available. Incidentally, the new term for this and other applications is “lumen-apposing metal stent” (LAMS).
Sometimes, however, the pendulum swings in the opposite direction; the same group that published the above-mentioned meta-analysis must be congratulated for performing the randomized trial that was recently completed. An interim report focusing on adverse events appeared last year, detailing a few severe complications, mainly involving bleeding, but also stent dislocation or luminal overgrowth by gastric mucosa, all after more than 2–3 weeks [4]. The study approach in the LAMS group was thereafter altered to include a shorter duration of metal stenting. This short report in Gut provoked quite a few letters reporting similar complications, not only with this metal stent but also with others [5–7]. However, the rate was not confirmed by other case series with lower complication rates, and with lower bleeding rates in particular [8–10]. However, a series in Spain including 211 patients with fully covered metal stents reported a higher rate of significant adverse events, independent of the metal stent type, at the level of 21% (with bleeding in 7%) [11].
A recently published larger retrospective comparative series including 103 patients, most of whom were treated with double-pigtail stents and only 19 of whom received LAMS, had a similar focus to that of the above-mentioned randomized trial. The efficacy was similar, but again the rate of complications was much higher in the LAMS group, as was the rate of unplanned repeat interventions [12].
In view of the high costs involved and a potentially higher complication rate, a final judgment on the best clinical indication for LAMS is still unclear on the basis of the mostly weak data that are currently appearing in the literature. The indications in these case series were also mixed. In the case of pancreatic cysts, the main issue is drainage, and LAMS might perhaps achieve this more quickly. In the case of WON, the first question is always whether this is really necrotic tissue to a certain extent, or fluid collections with some debris that could be equally drained. However, the therapeutic approach for WON involves not only drainage (often only partially successful), but also access for possible later interventions such as necrosectomy, etc. Initial enthusiastic reports often lead to counter-reactions, particularly in case of complications. Despite this, we should not draw the opposite conclusions, but rather wait for good, prospective, and also randomized data, and we should also contribute to the acquisition of the data needed in order to reach a fair and adequate assessment.
References
- Arvanitakis M, Delhaye M, Bali MA, et al. Pancreatic-fluid collections: a randomized controlled trial regarding stent removal after endoscopic transmural drainage. Gastrointestinal endoscopy 2007;65:609-19.
- Rodrigues-Pinto E, Baron TH. Evaluation of the AXIOS stent for the treatment of pancreatic fluid collections. Expert review of medical devices 2016;13:793-805.
- Bang JY, Hawes R, Bartolucci A, Varadarajulu S. Efficacy of metal and plastic stents for transmural drainage of pancreatic fluid collections: a systematic review. Digestive endoscopy : official journal of the Japan Gastroenterological Endoscopy Society 2015;27:486-98.
- Bang JY, Hasan M, Navaneethan U, Hawes R, Varadarajulu S. Lumen-apposing metal stents (LAMS) for pancreatic fluid collection (PFC) drainage: may not be business as usual. Gut 2016.
- Ryan BM, Venkatachalapathy SV, Huggett MT. Safety of lumen-apposing metal stents (LAMS) for pancreatic fluid collection drainage. Gut 2017;66:1530-1.
- Stecher SS, Simon P, Friesecke S, et al. Delayed severe bleeding complications after treatment of pancreatic fluid collections with lumen-apposing metal stents. Gut 2017.
- Zhu H, Lin H, Jin Z, Du Y. Re-evaluation of the role of lumen-apposing metal stents (LAMS) for pancreatic fl uid collection drainage. Gut 2017.
- Yoo J, Yan L, Hasan R, Somalya S, Nieto J, Siddiqui AA. Feasibility, safety, and outcomes of a single-step endoscopic ultrasonography-guided drainage of pancreatic fluid collections without fluoroscopy using a novel electrocautery-enhanced lumen-apposing, self-expanding metal stent. Endoscopic ultrasound 2017;6:131-5.
- Siddiqui AA, Kowalski TE, Loren DE, et al. Fully covered self-expanding metal stents versus lumen-apposing fully covered self-expanding metal stent versus plastic stents for endoscopic drainage of pancreatic walled-off necrosis: clinical outcomes and success. Gastrointestinal endoscopy 2017;85:758-65.
- Walter D, Will U, Sanchez-Yague A, et al. A novel lumen-apposing metal stent for endoscopic ultrasound-guided drainage of pancreatic fluid collections: a prospective cohort study. Endoscopy 2015;47:63-7.
- Vazquez-Sequeiros E, Baron TH, Perez-Miranda M, et al. Evaluation of the short- and long-term effectiveness and safety of fully covered self-expandable metal stents for drainage of pancreatic fluid collections: results of a Spanish nationwide registry. Gastrointestinal endoscopy 2016;84:450-7.e2.
- Lang GD, Fritz C, Bhat T, et al. EUS-guided drainage of peripancreatic fluid collections with lumen-apposing metal stents and plastic double-pigtail stents: comparison of efficacy and adverse event rates. Gastrointestinal endoscopy 2017.