Empiric Prophylactic Plastic Stenting for Disconnected Pancreatic Duct After Necrosectomy Is Not Uniformly Beneficial
Bret T. Petersen, MD, MASGE, reviewing Chavan R, et al. Endoscopy 2022 Feb 18.
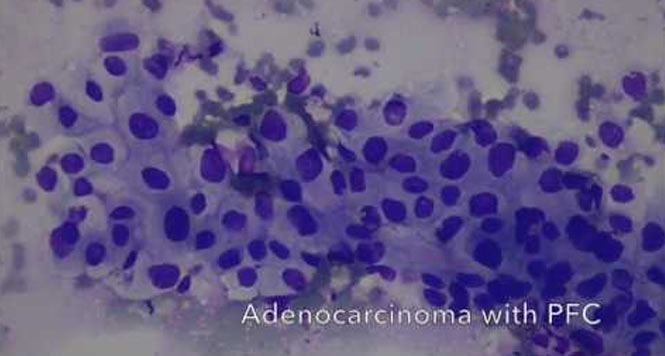
Pancreatic necrosis often results in main pancreatic duct injury and eventual discontinuity, or so-called disconnected pancreatic duct syndrome (DPDS), with recurrent symptoms from duct obstruction and/or recurrent pancreatic fluid collections (PFC). Some practices have resorted to leaving a transgastric double-pigtail stent in place long term after endoscopic decompression and resolution of walled-off necrosis (WON).
The authors of this study compared the recurrence of PFC at 3, 6, and 12 months among 104 patients with DPDS who were randomized to plastic stent placement (n=52) or no stent (n=52) upon completion of large-caliber stent drainage for WON. Metal stents were typically removed 4 weeks after initial drainage.
Plastic stents were successfully placed in 88.5% of patients and subsequently migrated in 19.2% of patients during 8 months of follow-up (median interquartile range, 2.5-12). Overall fluid collections recurred in 7 (13%) of the stented patients and 13 (25%) of the nonstented patients, which was not statistically different at 3, 6, and 12 months. Recurrent fluid collections following prophylactic stenting warranted repeat stenting in 1 patient and surgery in 2. Recurrence without prophylactic stenting required repeat EUS-guided stent placement in 4 patients.

COMMENTMost patients with DPDS after acute pancreatitis and endoscopic therapy of WON do not develop recurrent fluid collections. Although patients are highly prone to infection during the acute phase of necrosis, late recurrent fluid collections from DPDS tend to be less complex and can usually be managed with EUS-guided drainage when necessary. Thereafter, the small-caliber stents used for drainage of symptomatic recurrence can be left indefinitely.
Note to readers: At the time we reviewed this paper, its publisher noted that it was not in final form and that subsequent changes might be made.
CITATION(S)
Chavan R, Nabi Z, Lakhtakia S, et al. Impact of transmural plastic stent on recurrence of pancreatic fluid collection after metal stent removal in disconnected pancreatic duct: a randomized controlled trial. Endoscopy 2022 Feb 18. (Epub ahead of print) (https://doi.org/10.1055/a-1747-3283)