Paris Classification: Early Colorectal Cancers
Alexander Meining, Ulm; Thomas Rösch, Hamburg
The Paris classification for superficial / early tumors presented and discussed in the general section should be part of a standard terminology for endoscopic assessment. Figure shows the schematic presentation.
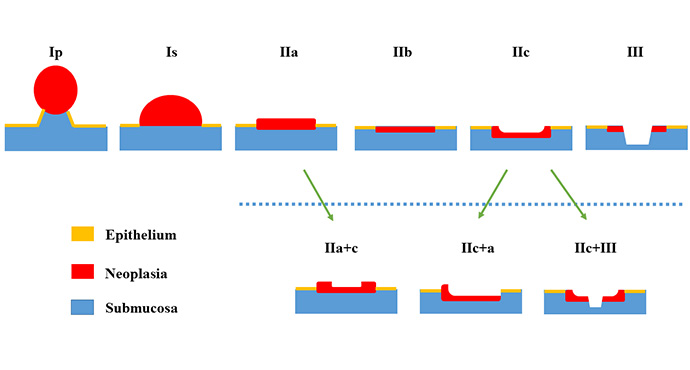
This classification applies to the entire gastrointestinal tract. In the colon, however, there are additional characteristics which must be taken into account. On the one hand, in contrast to the upper GI tract, a single resection can be regarded as curative, even if the submucosa is infiltrated up to 1,000 ?m and a so-called “low-risk” constellation is described (G1/2, L0, V0, R0). Furthermore, it should be noted that pT1 carcinomas in the colorectum always infiltrate the submucosa by definition. For mucosal carcinomas or pTis, the term “high-grade intraepithelial neoplasia / dysplasia” applies here.
It should also be considered that in the colon most lesions are adenomas (mostly tubulo / tubulo-villous with low-grade dysplasia). The size of the lesion plays an essential role in polypoid findings (Ip and Is) (although the Paris classification in the general sense only describes lesions less than 2 cm). Furthermore, in the colon, there is good evidence that not only the general appearance of the lesion, but also the surface structure of the mucosa should be appreciated in order to estimate the malignant potential of a lesion (see also www.endoscopy-campus.com/en/klassifikationen/nice-klassifikationen-zur-colonpolypen-differentialdiagnose/).
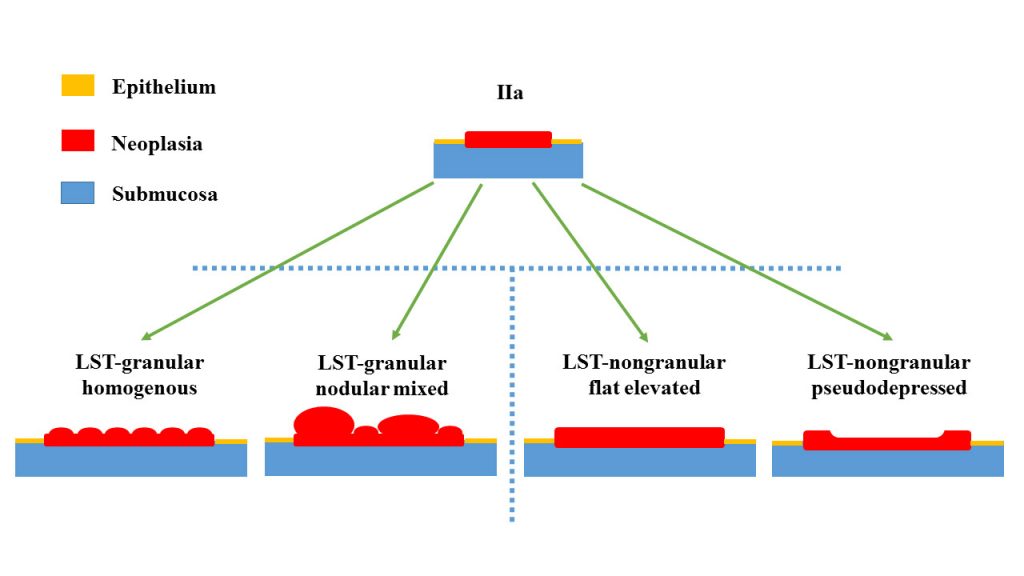
Last but not least, the so-called “lateral spreading tumors” (LST) must be taken into account as an additional subgroup of the type IIa lesions. This subgroup is subdivided again because different characteristics of the LSTs imply a different neoplastic potential and should therefore also be treated differently. LSTs are always larger than 2 cm (!) and are called “LST of granular-type” or “LST of non-granular type”. The group of “LST-granular homogenous” are the most common among these. Despite their sometimes considerable size, they almost always bear a low malignant potential (low grade dysplasia). In the case of the “nodular mixed type”, the size of the node probably plays a role, since in the case of nodular parts greater than 1 cm, a higher degree of neoplasia is frequently present. “Nongranular LSTs” bear a greater malignant potential. In several studies, the rates of submucosal invasive carcinomas in both forms are about 1–3% (granular) versus up to 15% (non-granular). Depressed non-granular lesions appear to bear the highest risk.
Figure shows Paris-Classification for the special case of colonic lesions with respect to the various types of lateral spreading tumors.
Here are some examples of the classification (including its limitations).
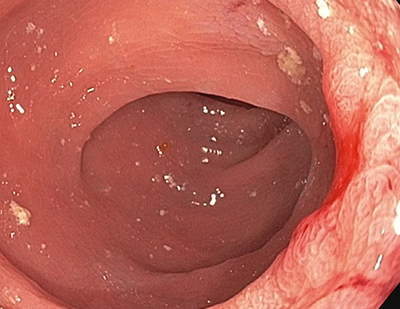
Example Colon 1: Type Ip
Example Colon 2: Type Is
Histology: No neoplasia, only hyperplasia! Taken a closer look at this Is+c (sessile lesion with smal central depression) helps to clearly identify a NICE-I pattern.
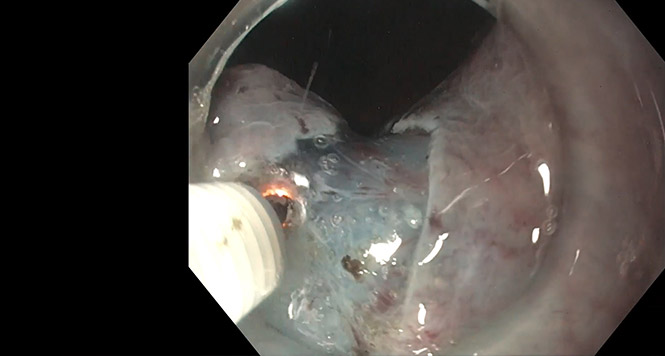
Example Colon 3: Type IIa
Histology: pT1 carcinoma with a high-risk constellation due to lymphatic vessel infiltration (left). pT1 carcinoma with a low-risk situation (right). Of interest, a “full-thickness resection” was performed on the left lesion, whereas oncological resection was performed on the right lesion due to the central depression (IIa + c). Different outcomes as expected. General appearance and pit pattern of both lesions are highly supsicious for cancerous lesions.
Example Colon 4: Type IIc
Histology: pT2-cancer! This has confirmed what our Japanese colleagues have postulated for a long time that (even relatively small) IIc lesions should primarily be surgically resected. In this case, endoscopic full-thickness resection was initially performed.
Example Colon 5: LST granular type
Histology: Low-grade IEN with focal high-grade IEN. The flat lesion covers half of the circumference with sessile components.
Histology: Low-grade IEN. This rectal lesion is so flat, that it is hardly visible with full insufflation (left side) and without NBI (right side, now more visible).
Histology: Two cases with low-grade IEN. The lesion on the right side covered 2/3 of the rectal circumference and had a length of 7 cm.
Example Colon 6: LST granular type, nodular-mixed
Histology: pT1-carcinoma with low-risk criteria (endoscopic R0 resection), quite similar to the lesion in example 5, left side, but with a larger nodule. Using the LCI mode (see also www.endoscopy-campus.com/lehrvideo/endoskopische-diagnostik-von-colonpolypen-anhand-der-nice-klassifikation/ ) centrally an increased vascularisation and an interruption of the mucosal structure is seen, which is a hallmark of an advanced neoplasia.
Histology: Tubulo-villous adenoma with focal high-grade IEN. Large lesion area (more than 2/3 of the circumference). The larger nodular part is seen on the right side.
Example Colon 7: LST nongranular type
Histology: Similar picture as above in the NBI zoom mode pathologic vessels (right side). On histology only low-grade EIN.
Example Colon 8: LST nongranular type, pseudodepressed
Histology: Both lesions with high-grade IEN. The lesion on the left shows a nodular component at 8h, which may suggest “LST granular type, nodular-mixed”. The central part fulfills the criteria of a “LST nongranular, pseudodepressed”.