BING Classification Early Barrett Neoplasia
Dominic Brookman-Amissah und Oliver Pech, Regensburg
Multimodal therapy for early Barrett’sneoplasias (endoscopic resection of all visible neoplasias, followed byablative treatment for residual nondysplastic Barrett’s mucosa), has becomeestablished as the standard therapy and is set out in national andinternational guidelines. These dysplastic lesions continue to be difficult todetect. Discrete dysplastic mucosal changes are often very small, flat (ParisIIb), and irregular in appearance, so that they are frequently not recognized.In addition, the monitoring protocols that have been recommended to date, withfour-quadrant biopsies (e.g., using the Seattle protocol) and high-resolution (HR)white-light endoscopy, cover only 4–5% of the total surface of the Barrett’smucosa. Most of the Barrett’s epithelium is therefore not examined [1].
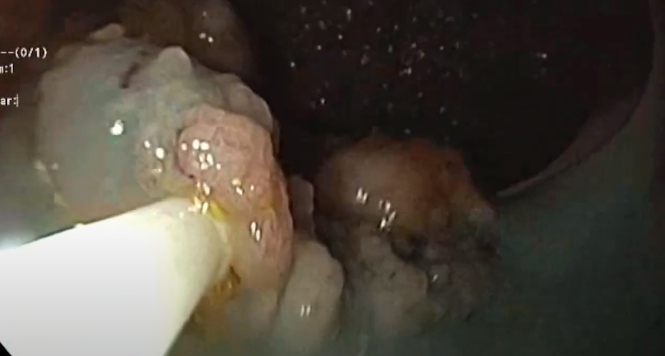
In comparison with pure white-lightendoscopy, the narrow-band imaging (NBI) mode allows much better differentiation,particularly of flat, discrete mucosal changes and their extent within anotherwise homogeneous area of intestinal metaplasia [2].
In 2016, the Barrett’s International NBI Group (BING) (including committees of experts on Barrett’s from the USA, Europe, and Japan: University of Kansas, University of Chicago, Academic Medical Center in Amsterdam, University of Augsburg, Hokkaido University, and Jikei University) developed a classification for identifying dysplastic areas and early carcinomas inside Barrett’s mucosa using NBI.
According to this BING classification, there are changes that occur in the mucosal surface pattern and in the mucosal vascular architecture during the development of dysplasia and early neoplasia — in contrast to nondysplastic Barrett’s esophagus (NDBE) (Table 1). This validated classification can be used for histopathological prediction of the presence of possible high-grade dysplasia or early carcinoma within these often flat, poorly detectable areas.
The research group’s evaluation, with substantial interobserver agreement (? = 0.681), showed high rates of accuracy (92%), sensitivity (91%), and specificity (93%), as well as a high positive predictive value (89%) and negative predictive value (95%) [3,4].
Consensus-based NBI classification of Barrett’s epithelium
| Morphological characteristics | Classification |
|---|---|
| Mucosal surface | |
| Circular villous/gyrate or tubular surface pattern | Regular |
| Absence of the above characteristics, or irregular mucosal pattern | Irregular |
| Mucosal vascular architecture | |
| Vessels directed regularly along the mucosal pattern, with normal, longitudinal branching | Regular |
| Focally or diffusely distributed, elongated, corkscrew-like, with the course not following the mucosa, short and irregularly branched | Irregular |





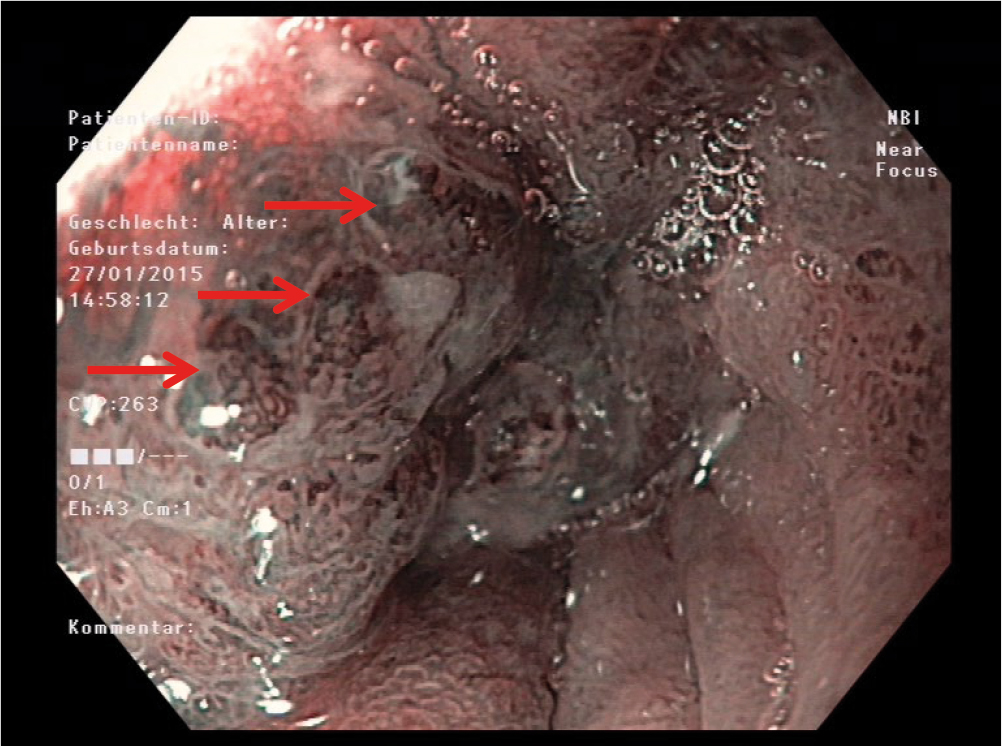

With targeted biopsies, NBI-supported mucosal assessment significantly improves the detection rate for dysplastic and early neoplastic Barrett’s mucosa, and it should be used in addition to four-quadrant biopsies.
References:
- Koop H et al. S2k-Leitlinie: GastroösophagealeRefluxkrankkheit, Z Gastroenterol 2014; 52: 1299–1346
- Levine DSet al. Safety of a systenmatic endoscopic biopsy protocol in patients withBarrett`s esophagus, Am J Gastroenterol2000; 95: 1152–7
- Sharma Pet al. Standard endoscopy with random biopsies versus narrow band imagingtargeted biopsies in Barrett`s oesophagus: a prospective, international,randomized controlled trial, Gut 2013; 62:15–21
- Sharma Pet al. Development and validation of a classification system to identify highgrade dysplasia and esophageal adenocarcinoma in Barrett`s esophagus usingnarrow band imaging, Gastroenterology 2016; 150:591–598