The “black” esophagus
Wladyslaw Januszewicz, Warsaw, Poland
Department of Gastroenterology, Hepatology and Clinical Oncology, Medical Centre for Postgraduate Education, Warsaw, Poland
A 68-year old woman with advanced endometrial cancer and evidence of methicillin-resistant Staphylococcus aureus (MRSA) bacteremia and cytomegalovirus (CMV) infection was referred to endoscopy unit with suspicion of upper gastrointestinal (UGI) bleeding.
For six days before presentation the patient had been staying within the oncological ward for evaluation of endometrial cancer. Her past medical history included ischemic heart disease, essential hypertension, hypothyroidism and acute pancreatitis of unknown origin. Due to comorbidities and advanced loco-regional involvement of the disease, she was found to be ineligible for surgical treatment. During her stay in the ward, as she was being prepared for palliative chemotherapy, her condition deteriorated, and she developed a hectic fever and acute renal failure with evidence of central venous catheter-related MRSA infection and vesicovaginal fistula. Moreover, due to significant weight loss, loss of appetite, and nausea she was placed on total parenteral feeding. On the day before presentation she had an episode of a non-cardiac chest pain, coffee-ground emesis, passage of black stool and a decrease in haemoglobin level from 14.5 g/dl to 12.3 g/dl. With suspicion of UGI bleeding, she was referred for esophagogastroduodenoscopy (EGD), which showed a circumferential black discoloration of the esophagus with a sharp transition to normal mucosa at the gastroesophageal junction; findings which were consistent with acute esophageal necrosis (AEN).
AEN, also known as the “black esophagus,” was first described in the early 1990s (1) and characterizes a rare clinical condition with a prevalence of approximately 0.3% (2). AEN is more common in elderly males and usually presents itself with UGI bleeding (3). The diagnosis is made endoscopically through visual identification of diffuse circumferential black discoloration of esophageal mucosa affecting mostly the distal esophagus with a sharp transition to a normal lining at the gastroesophageal junction. AEN is related with a high mortality rate of ~12.5 %, which is usually due to underlying conditions (3). The most common long-term complication is a stricture formation, which may occur in up to 25% of cases (3). The pathophysiology of AEN is most likely multifactorial and is a combination of ischemic insult, compromised mucosal defences, and corrosive injury due to the reflux of the gastric contents (4). Infectious causes have also been postulated, including cytomegalovirus (CMV) infection (5). This was most likely the case in the presented patient as the day after the endoscopy her blood samples showed a high viral load of CMV on polymerase chain reaction (PCR) assay. She was kept nil-per-os, started on aggressive resuscitation with i.v. fluids, and received proton-pump inhibitors. She continued a course of broad-spectrum antibiotics and was given ganciclovir i.v. for CMV infection. She remained afebrile in a stable condition for the next week and was moved to a home hospice care near her place of residence for continuation of treatment.
Figure legend
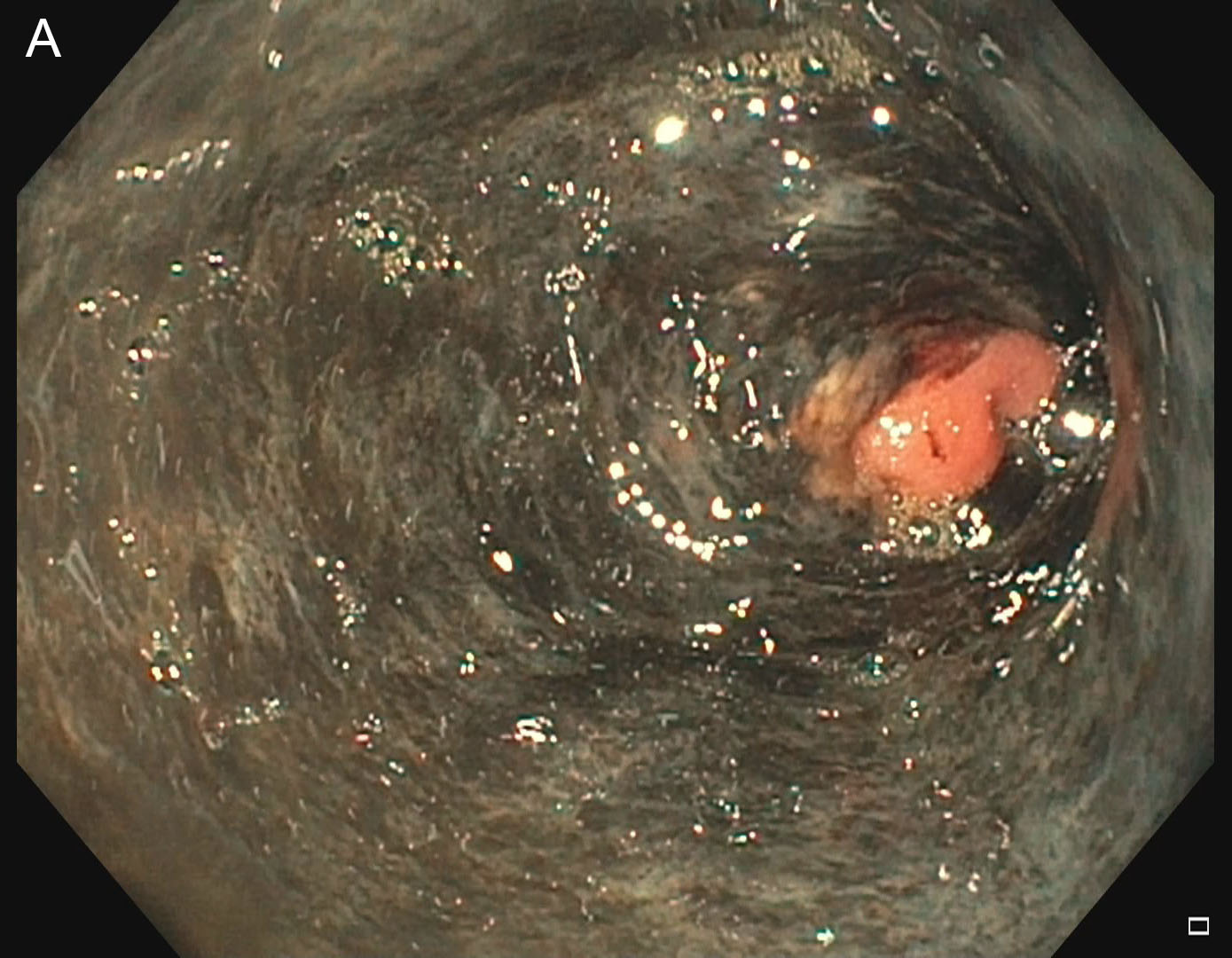
Endoscopic images showing a diffuse black discoloration of the necrotic mucosa in the distal esophagus, with a sharp transition to normal epithelium at the gastroesophageal junction (A).The changes are still visible in the mid-esophagus (B) and less profound in the proximal esophagus (C).
References:
1. Goldenberg SP, Wain SL, Marignani P. Acute necrotizing esophagitis. Gastroenterology. 1990 Feb 1;98(2):493–6.
2. Vohra I, Attar B, Almoghrabi A. Black Esophagus: Acute Esophageal Necrosis. Clin Gastroenterol Hepatol. 2020 [Epub ahead of print].
3. Gurvits GE, Cherian K, Shami MN, Korabathina R, El-Nader EMA, Rayapudi K, et al. Black Esophagus: New Insights and Multicenter International Experience in 2014. Dig Dis Sci. 2015 Jan 23;60(2):444–53.
4. Gurvits GE. Black esophagus: Acute esophageal necrosis syndrome [Internet]. Vol. 16, World Journal of Gastroenterology. Baishideng Publishing Group Inc.; 2010 [cited 2020 May 10]. p. 3219–25. Available from: http://www.wjgnet.com/1007-9327/full/v16/i26/3219.htm
5. Trappe R, Pohl H, Forberger A, Schindler R, Reinke P. Acute esophageal necrosis (black esophagus) in the renal transplant recipient: manifestation of primary cytomegalovirus infection. Transpl Infect Dis [Internet]. 2007 Mar 1 [cited 2020 May 10];9(1):42–5. Available from: http://doi.wiley.com/10.1111/j.1399-3062.2006.00158.x