First Results from the NordICC randomized trial on screening colonoscopy
Thomas Rösch, Hamburg
JAMA Intern Med. 2016 May 23. doi: 10.1001/jamainternmed. 2016.0960. [Epub ahead of print]
| Original Investigation Population-Based Colonoscopy Screening for Colorectal Cancer A Randomized Clinical Trial |
| Michael Bretthauer, MD; Michal F. Kaminski, MD; Magnus Løberg, MD; Ann G. Zauber, PhD; Jaroslaw Regula, MD; Ernst J. Kuipers, MD; Miguel A. Hernán, MD; Eleanor MC Fadden, MA; Annike Sunde, MSc; Mette Kalager, MD; Evelien Decker, MD; Iris Lands-dorp-Vogelaar, PhD; Kjetil Garborg, MD; Maciej Rupinski, MD; Manon C. W. Spaander, MD; Marek Bugajski, MD; Ole Høje, MD; Tryggvi Stafansson, MD; Geir Hoff, MD; Hans-Olov Adami, MD; for the Nordic-European Initiative on Colorectal Cancer (NordICC) Study Group |
ABSTRACT
Importance
Although some countries have implemented widespread colonoscopy screening, most European countries have not introduced it because of uncertainty regarding partici-pation rates, procedure-related pain and discomfort, endoscopist performance, and effectiveness. To our knowledge, no randomized trials on colonoscopy screening cur-rently exist.
Objective
To investigate participation rate, adenoma yield, performance, and adverse events of population-based colonoscopy screening in several European countries.
Design, Setting, and Population
A population-based randomized clinical trial was conducted among 94 959 men and women aged 55 to 64 years of average risk for colon cancer in Poland, Norway, the Netherlands, and Sweden from June 8, 2009, to June 23, 2014.
Interventions
Colonoscopy screening or no screening.
Main Outcomes and Measures
Participation in colonoscopy screening, cancer and adenoma yield, and participant experience. Study outcomes were compared by country and endoscopist.
Results
Of 31 420 eligible participants randomized to the colonoscopy group, 12 574 (40.0%) underwent screening. Participation rates were 60.7%in Norway (5354 of 8816), 39.8%in Sweden (486 of 1222), 33.0%in Poland (6004 of 18 188), and 22.9% in the Netherlands (730 of 3194) (P < .001). The cecum intubation rate was 97.2%(12 217 of 12 574), with 9726 participants (77.4%) not receiving sedation. Of the 12 574 participants undergoing colonoscopy screening, we observed 1 perforation (0.01%), 2 postpolypectomy serosal burns (0.02%), and 18 cases of bleeding owing to poly-pectomy (0.14%). Sixty-two individuals (0.5%) were diagnosed with colorectal cancer and 3861 (30.7%) had adenomas, of which 1304 (10.4%) were high-risk adenomas. Detection rates were similar in the proximal and distal colon. Performance differed significantly between endoscopists; recommended benchmarks for cecal intubation (95%) and adenoma detection (25%) were not met by 6 (17.1%) and 10 of 35 endosco-pists (28.6%), respectively. Moderate or severe abdominal pain after colonoscopy was reported by 601 of 3611 participants (16.7%) examined with standard air insufflation vs 214 of 5144 participants (4.2%) examined with carbon dioxide (CO2) insufflation (P < .001).
Conclusions and Relevance
Colonoscopy screening entails high detection rates in the proximal and distal colon. Participation rates and endoscopist performance vary significantly. Postprocedure ab-dominal pain is common with standard air insufflation and can be significantly reduced by using CO2.
What you should know about this paper
Screening colonoscopy is well established in a few Western countries as primary method of colorectal cancer (CRC) screening; however, most Western countries use conventional (FOBT) or immunologic stool tests (FIT), and there is no evidence from randomized trials to support colonoscopy as primary CRC screening test. This evidence is available from multiple randomized trials for fecal occult blood test (FOBT) and for flexible sigmoidoscopy (FS)1-3.
For both screening tests, a recent metaanalysis1 shows the following with regards to risk reduction by the test
| Test | no of studies | Risk reduction in CRC incidence |
CRC mortality | overall mortality |
|---|---|---|---|---|
| FOBT | 4 | 0.95 | 0.87 | 1.00 |
| FS | 5 | 0.82 | 0.72 | 0.98 |
These are the benchmark values any test has to fulfill and/or surpass in order to be in the game long-term. Colonoscopy has only be analyzed in a multitude of non-randomized trials, mostly retrospective, many of them as case-control studies, and some positive effects were claimed2. To arrive at a higher evidence levels, there are three randomized trial underway, two comparing fecal immunochemical testing (FIT) with colonoscopy – COLOPREV4 and CONFIRM (Clinical Trials.gov Identifier: NCT01239082). The third study is at least equally important for colonoscopists, since it randomizes colonoscopy to no screening in a 2:1 relationship5.
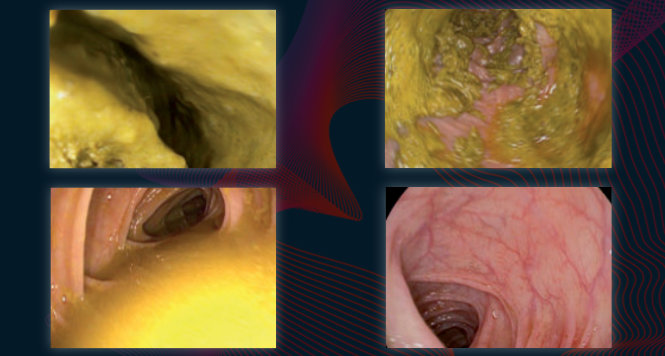
The present paper is the first analysis of the NordICC randomized trial performed in Sweden, Norway, Netherlands and Poland, comparing colonoscopy with no screening. Of the 94959 individuals included in the entire study, a third was randomized to the colonoscopy arm; 12574 accepted to undergo the test (40%). These rates were highest in Norway (60%), still quite good in Poland and Sweden (333 and 40%), and much lower in the Netherlands (23%). Candidates were invited once with a letter and an information leaflet. Trial endoscopists had to have experience of at least 300 colonoscopies and do an annual workload of 200 colonoscopies.
The study reports on the yield of neoplasia: With a cecal intubation rate of 97.2%, rates for CRC, all adenomas and advanced adenomas were 0.5%, 30.7% and 10.4%, respectively. These rates were of course variable between endosopists and benchmarks for complete colonoscopy (95%) and adenoma detection rate (25%) were not met by 17% and almost 30% of colonoscopists. This is remarkable, and leaves some questions open for the final study outcome; previous studies have clearly shown that adenoma detection rates (ADR) below 20% were associated with significantly more missed (or interval) cancers6; the cut-off rates for interval cancers which was 20% in that study was more recently moved upwards by a US study claiming that the interval cancer rates were directly correlated with ADR up to an adenoma detection rate of 52%; with each 1% in ADR increase a 3% decrease in interval cancers was found7. If in 30% of colonoscopists in this study, ADR is too low – what does that mean for the study results with regards to the reduction of CRC incidence and mortality ?
Three quarters of screenees (77.4%) did not receive sedation; the rates of moderate to severe post-colonoscopy pain was significantly lower with the use of CO2 (4.2%) than with room air (16.7%). This practice of non-sedation may be typical for northern countries, but is certainly not representative for Germany, France and southern countries. CO2 for colonoscopy on the other hand is well established by a large number of randomized trial all showing a superiority of C02 with regards to patient discomfort8, so here, the study results are confirmatory.
The study sheds a first light on what we might expect from this extremely important randomized trial which will not be available before 2020; neoplasia rates are comparable to German programme and slightly higher than reported from the Polish programme years ago. The challenge will be to show CRC incidence and mortality reduction to a larger extent than demonstrated in prior screening trails, e.g. when using simoidoscopy. So, colonoscopists, lets keep our fingers crossed!
Literature
- Holme O, Bretthauer M, Fretheim A, et al. Flexible sigmoidoscopy versus faecal occult blood testing for colorectal cancer screening in asymptomatic individuals. Cochrane Database Syst Rev 2013;9:Cd009259.
- Brenner H, Stock C, Hoffmeister M. Effect of screening sigmoidoscopy and screening colonoscopy on colorectal cancer incidence and mortality: systematic review and meta-analysis of randomised controlled trials and observational studies. Bmj 2014;348:g2467.
- Heresbach D, Manfredi S, D‘Halluin P N, et al. Review in depth and meta-analysis of controlled trials on colorectal cancer screening by faecal occult blood test. Eur J Gastroenterol Hepatol 2006;18:427-33.
- Quintero E, Castells A, Bujanda L, et al. Colonoscopy versus fecal immunochemical testing in colorectal-cancer screening. N Engl J Med 2012;366:697-706.
- Kaminski MF, Bretthauer M, Zauber AG, et al. The NordICC Study: rationale and design of a randomized trial on colonoscopy screening for colorectal cancer. Endoscopy 2012;44:695-702.
- Kaminski MF, Regula J, Kraszewska E, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med 2010;362:1795-803.
- Corley DA, Jensen CD, Marks AR, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 2014;370:1298-306.
- Sajid, Caswell J, Bhatti M, et al. Carbon dioxide insufflation versus conventional air insufflation for colonoscopy: a systematic review and meta-analysis of published randomized controlled trials. Colorectal Dis 2014.